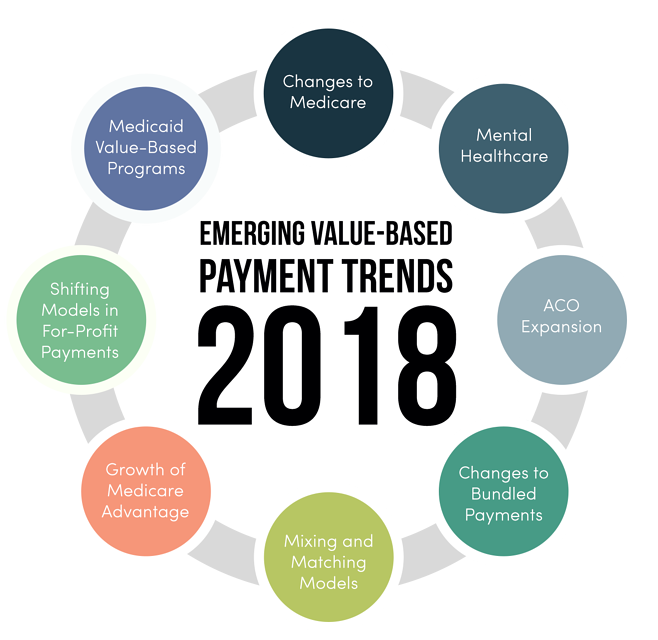
As uncertainty regarding the future of the nation's healthcare laws and payment structures continue into 2018, hospitals and other providers are planning to intensify their focus on quality care delivery and payment innovation. While this trend has been ongoing for more than a decade in localities throughout the country, new reforms in public and private payment models are forcing providers to refocus their efforts. Here are some of the trends in 2018 that will have the biggest impact.
Changes to Medicare
During the past few years, the Medicare system has pushed value-based care through several different payment models, both mandatory and voluntary. With fresh leadership in the Department of Health and Human Services, the mandatory models are expected to be dropped and the voluntary ones emphasized. In 2017, non-exempted physicians paid through Part B were forced to choose between Merit-based Incentive Payment System (MIPS) or a choice of advanced alternative payment models (APMs). In 2018, more providers are expected to go with APMs. Medicare accounts for 20% of all national health expenditures, so providers must pay attention to payment changes if they plan on maximizing their revenue.
Mental Healthcare
One APM that doctors are expected to move to in 2018 is Comprehensive Primary Care Plus (CPC+). A critical component of this initiative is a focus on integrated mental health care. This is likely to be a major challenge for providers because of the shortage of mental health professionals, specifically psychiatrists, throughout the country. More patients than ever are covered for mental health services because of the Affordable Care Act, but the shortage of mental health personnel in private practices and outpatient centers has caused patients to go to emergency rooms for care, causing a spike in costs. Providers will need to put more emphasis on value-based mental health care delivery to take full advantage of CPC+ and other models.
ACO Expansion
In order to deliver high-quality care and adhere to Medicare payment models managed by the Centers for Medicare & Medicaid Services (CMS), physicians, hospitals and other providers form voluntary groups known as accountable care organizations (ACO). In 2018, experts are expecting to see a big spike in the formation of these ACOs. There are several different models available for these organizations, including:
- Medicare Shared Savings Program
- Advanced Payment ACO Model
- Pioneer ACO Model
In previous years, ACOs faced a wide range of challenges, causing more than 100 of them to drop out of both Medicare and commercial plans. New organizations formed in 2018 will need to find better ways to engage physicians in payment models and make sure that staff are truly focused on making improvements to value-based care delivery.
Changes to Bundled Payments
The shift from mandatory to voluntary participation in bundled payment models is expected to continue throughout 2018. Late in 2017, CMS cancelled mandatory programs for hip replacement as well as for cardiac care and cardiac rehabilitation. These cancelled programs will most likely be replaced by a large voluntary program known as Bundled Payments for Care Improvement (BPCI) and maybe some additional models. Providers who have seen success through gain-sharing and other aspects of the now cancelled bundled payment plans will most likely continue to see success in voluntary models because of their focus on value-based care.
Mixing and Matching Models
The lessons learned by doctors, hospitals and other providers in recent years through participation in voluntary and mandatory models can be used in interesting ways in 2018 and beyond. ACOs are starting to mix and match successful payment and care-delivery methods while moving away from one-size-fits-all programs. A Colorado-based health provider is successfully using mixing and matching by implementing a Virtually Integrated Care Team. The program has reduced length of visits, readmission rates, response times, and per-hour patient costs. Both high and low-tech innovations in value-based care are likely to be found through careful analysis of existing payment data.
Growth of Medicare Advantage
The private payer arm of Medicare, known as Medicare Advantage or Medicare Part C, is likely to see a lot of growth in 2018 as the Trump administration and congress continue to carry out their plans for increased privatization of government services. This could come with many advantages for healthcare providers, including:
- Lower costs through enhanced collaboration
- Improved patient access to services
- Better outcomes through data sharing
At the beginning of 2018, about 34% of Medicare enrollees were covered by Medicare Advantage. That figure is expected to rise to over 50% by the end of the decade. The success of Medicare Advantage will depend on getting high star ratings through value-based care delivery.
Shifting Models in For-Profit Payments
CMS and other non-profit organizations aren't the only payers shifting focus to value-based payment models. Large, high profit insurance companies like Blue Cross are now including payment incentives that are encouraging providers to focus on team-based care with greater participation from nurses and clinical social workers. Since a majority of people in the United States are still covered by private commercial plans, this shift towards value-based care can have significant impacts on a lot of lives. In 2018, more value-based relationships are expected to be formed between providers and the biggest for-profit payers.
Medicaid Value-Based Programs
During 2017, 40 states implemented reforms to the delivery systems of their Medicaid programs, and a majority of those states plan to expand or introduce new initiatives in 2018. Many Medicaid programs are taking a very different approach to value-based care by focusing more resources on life outside the walls of hospitals and private practices. This involves hiring more social workers and using technology to evaluate social factors that affect individual health. Medicaid bundled payment plans in many states also include maternity care and chronic health issues.
Every healthcare provider will be affected by 2018's trends in different ways, but one certainty is that each doctor or organization will need to improve patient outcomes while making cost improvements in order to be successful.
